You should divide the text into sentences and correct any mistakes. Here is the corrected version: You incomplete files, errors, high data acquisition fees, manual processes, redundant requests, variations, and requirements, as well as long lead times. Health plans and providers both face systemic challenges when it comes to credentialing and primary source verification. Verified by CA qh mncq, a certified credentials verification organization, fills the gap in primary source verification for health and dental plans. Verified improves the speed, integrity, and quality of the credentialing verification process, helping to eliminate redundancy, reduce turnaround time, and improve service across the industry. Direct integration with CA qh pro view enables immediate access to self-reported provider data, and automated integration with many primary sources also reduces the time required to conduct PSV. A rules-based decision-making engine reduces human error, with verified output delivered in human-readable as well as machine-readable form, enabling health plans to automatically feed this information into their provider data management systems. data elements in each file are categorized based on verification outcome so the plan can automatically route the file into the correct work queue. Verified also provides a comprehensive report of the conducted outreach, faster turnaround, higher quality, increased efficiency, and lower cost credentialing. Just got easier with verified. To learn more, please contact us today.
Award-winning PDF software





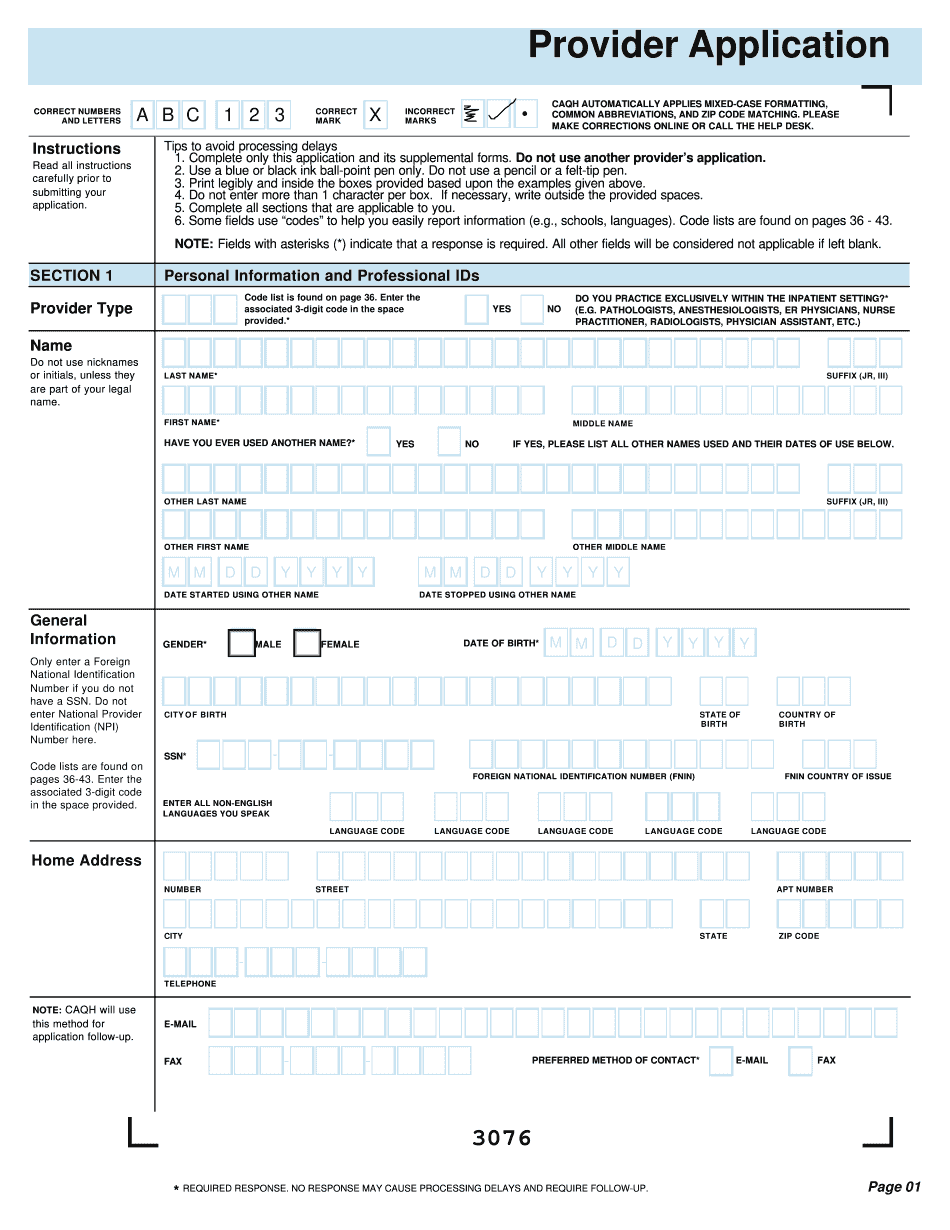
Caqh Solutions proview Form: What You Should Know
CASH will use the Medicare and Medicaid databases only to obtain your CASH Client ID (CPI). This information is required when submitting and processing your claims. CASH Client Information Form You can download an online Client Information Form. You only need to submit a short application and CASH Client Form. You are only required to complete the Client Information Forms once per year.
online solutions help you to manage your record administration along with raise the efficiency of the workflows. Stick to the fast guide to do Caqh Provider Application, steer clear of blunders along with furnish it in a timely manner:
How to complete any Caqh Provider Application online: - On the site with all the document, click on Begin immediately along with complete for the editor.
- Use your indications to submit established track record areas.
- Add your own info and speak to data.
- Make sure that you enter correct details and numbers throughout suitable areas.
- Very carefully confirm the content of the form as well as grammar along with punctuational.
- Navigate to Support area when you have questions or perhaps handle our assistance team.
- Place an electronic digital unique in your Caqh Provider Application by using Sign Device.
- After the form is fully gone, media Completed.
- Deliver the particular prepared document by way of electronic mail or facsimile, art print it out or perhaps reduce the gadget.
PDF editor permits you to help make changes to your Caqh Provider Application from the internet connected gadget, personalize it based on your requirements, indicator this in electronic format and also disperse differently.
Video instructions and help with filling out and completing Caqh Solutions proview