Award-winning PDF software





What does Caqh stand for Form: What You Should Know
CASH Credentialing Process. How does CASH offer a Credentialing Process? The Credentialing Process is a simple and secure process to certify new cardholders. CASH's credentialing platform provides a secure way for medical professionals as well as individuals interested in becoming How many people need a credentialing process? The Council for Affordable Quality Healthcare, Inc's data repository is expected to support millions of credentialing requests on behalf of many more Who can register for the credentialing service? All doctors who: Credential the provider to participate in the Council's marketplace as well as on the Council's electronic health records platform with an ID (e.g., CASH-Provider-Eligibility.pdf). The Council of Affordable Quality Healthcare, Inc What types of providers can be credentialed? Credential the provider to participate in the Council's marketplace as well as on the Council's electronic health records platform with an ID (e.g., What will happen when a doctor registers as a credentialed? The Council for Affordable Quality Healthcare, Inc's database will automatically search the provider's files to pull up any clinical data that the doctor may have. If the doctor wants to keep this data private, or wants to remove himself as a participant, he/she can do so. The Council for Affordable Quality Healthcare, Inc's database will automatically search the provider's files to pull up any clinical data that the doctor may How long will it take to receive a credential? An entire medical professional's medical chart will typically be entered within one to two days. How will the clinician know when it is time to log off of the site to take the next credentialing step? Once a credential has been uploaded to CASH, the clinician will receive an alert. This is a one-time message, so the clinician must take action when it occurs. What happens if the clinician does not get the credential he or she is wanting? The clinician will remain logged into CASH until the credential is processed. In these situations, it may take five business days to receive a credentialing response. What happens if a credentialing request is not completed within the five days? The clinician will have to return to CASH for the credentials.
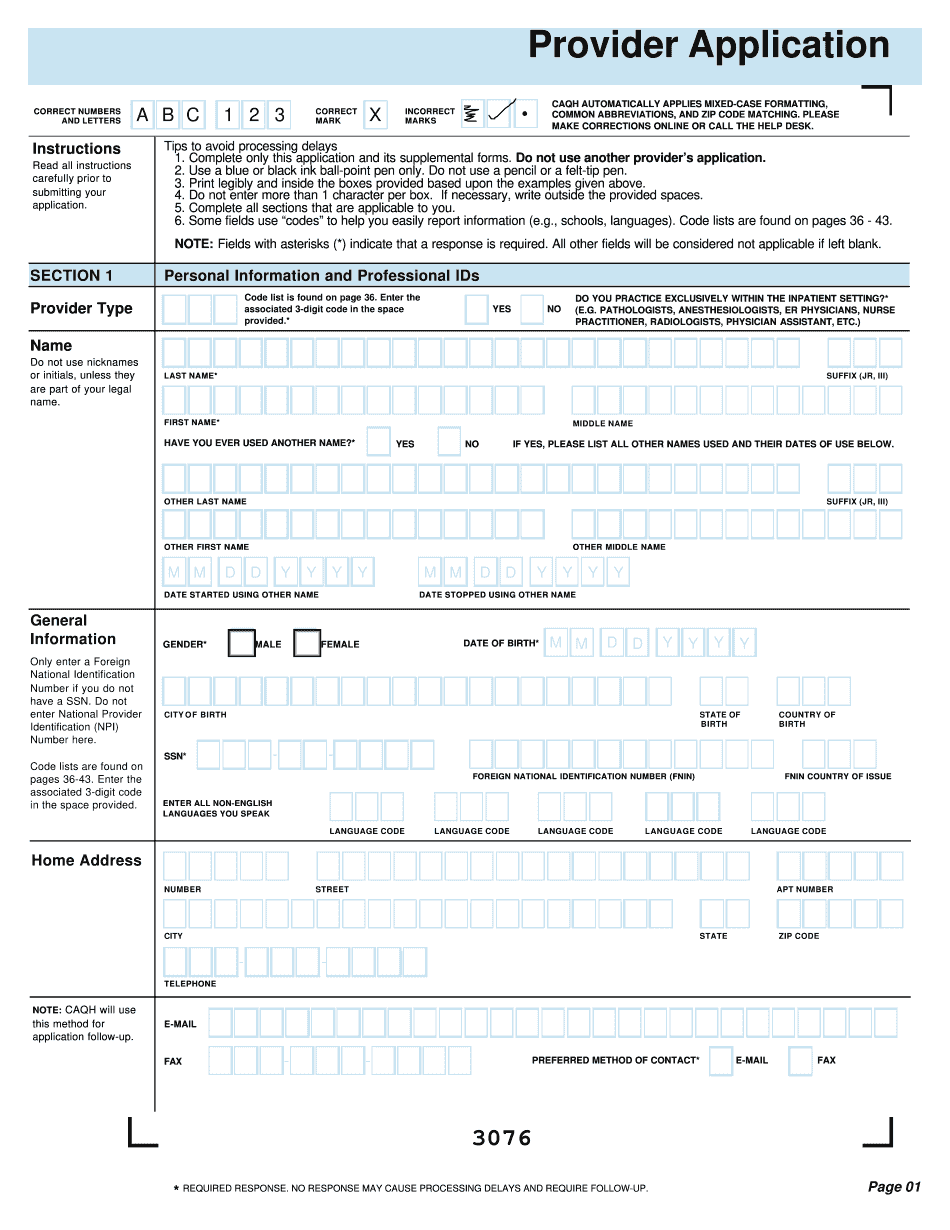
online solutions help you to manage your record administration along with raise the efficiency of the workflows. Stick to the fast guide to do Caqh Provider Application, steer clear of blunders along with furnish it in a timely manner:
How to complete any Caqh Provider Application online: - On the site with all the document, click on Begin immediately along with complete for the editor.
- Use your indications to submit established track record areas.
- Add your own info and speak to data.
- Make sure that you enter correct details and numbers throughout suitable areas.
- Very carefully confirm the content of the form as well as grammar along with punctuational.
- Navigate to Support area when you have questions or perhaps handle our assistance team.
- Place an electronic digital unique in your Caqh Provider Application by using Sign Device.
- After the form is fully gone, media Completed.
- Deliver the particular prepared document by way of electronic mail or facsimile, art print it out or perhaps reduce the gadget.
PDF editor permits you to help make changes to your Caqh Provider Application from the internet connected gadget, personalize it based on your requirements, indicator this in electronic format and also disperse differently.